National Birth Defects Prevention Study (NBDPS) Notable Studies 2007–2014
- Polycyclic Aromatic Hydrocarbons and Oral Clefts
- Butalbital Use and Birth Defects
- Antiherpetic Medication and Gastroschisis
- Genetics and Congenital Heart Defects
- Fever in Pregnancy and Congenital Heart Defects
- Air Pollution and Congenital Heart Defects
- The Potential Impact of Newborn Pulse Oximetry Screening
- Risk Factors for Choanal Atresia in the NBDPS
- Participation in the Genetic Component of NBDPS
- Obesity as a Risk Factor for Birth Defects
- Antidepressant Medications and Birth Defects
- Diet Quality and Neural Tube Defects (NTDs) and Orofacial Clefts
- Cooking and Grilling By-Products as a Risk Factor for Gastroschisis
- Folic Acid and Diabetes Associated Birth Defects
- Neural Tube Defects (NTDs) and Folate Intake among Pregnancies Conceived after Folic Acid Fortification in the United States
- Exposures during a Father’s Job and Birth Defects
To date, more than 300 scientific papers have been published using data from NBDPS. Some examples of important findings:
Polycyclic Aromatic Hydrocarbons and Oral Clefts
Polycyclic aromatic hydrocarbons (PAHs) are chemicals formed during the burning of coal, oil, gas, garbage, or from smoking cigarettes, cigars, or pipes, or from charbroiling meat. There are many ways to come in contact with PAHs at home or at work. NBDPS researchers looked for evidence of a link between PAHs in a woman’s workplace and oral clefts (clefts of the lip and palate) in their babies.
Among women interviewed for the NBDPS, researchers found that it was not very common for women to work in places with PAHs. PAH exposure occurred most often among women working in food preparation and serving. Pregnant women who worked in places with any PAHs were more likely to have babies with cleft lip with or without a cleft palate. Pregnant women who worked in places with higher PAH levels were even more likely to have babies with cleft lip than women who worked in areas with lower PAH levels. Since this was the first study to show this link, more research is needed to understand it fully.
Langlois PH, Hoyt AT, Lupo PJ, Lawson CC, Waters MA, Desrosiers TA, Shaw GM, Romitti PA, Lammer EJ. Maternal occupational exposure to polycyclic aromatic hydrocarbons and risk of oral cleft-affected pregnancies. Cleft Palate Craniofac J. 2013 May;50(3):337-46.

Butalbital Use and Birth Defects
Butalbital (byoo-TAL-bi-tal) is an ingredient in some medicines (for example, Fioricet®, Fiorinal®) prescribed for the treatment of migraine and tension-type headaches. Little is known about the safety or risk of using butalbital while pregnant. NBDPS researchers looked to see if there is a link between butalbital use and birth defects.
Researchers found that butalbital use is rare among women in NBDPS. Researchers also found a link between using butalbital while pregnant and certain congenital heart defects. The heart defects in the study with this link include tetralogy of Fallot, pulmonary valve stenosis, and atrial septal defects. This study is the first to show these links. More research is needed to learn more about the risks and benefits of butalbital use among pregnant women.
Browne ML, Van Zutphen AR, Botto LD, Louik C, Richardson S, Druschel CM; National Birth Defect Prevention Study. Maternal butalbital use and selected defects in the National Birth Defects Prevention Study. Headache. 2014 Jan;54(1):54-66.
Antiherpetic Medication and Gastroschisis
Gastroschisis is a birth defect of the abdominal (belly) wall. The baby’s intestines are outside of the baby’s body through a hole beside the belly button. The causes of gastroschisis are not known, but it is thought that exposures in early pregnancy might play a key role.
Herpes infections can occur during pregnancy, and to treat these infections antiherpetic medicines are sometimes used. Researchers used NBDPS data to see if antiherpetic medicine use in early pregnancy is linked to the risk of gastroschisis. This study found that the risk of gastroschisis could be higher in children born to women with herpes infection who used antiherpetic medicine. More research is needed to determine the risks of herpes and antiherpetic medications in pregnancy.
Ahrens KA, Anderka MT, Feldkamp ML, Canfield MA, Mitchell AA, Werler MM; National Birth Defects Prevention Study. Antiherpetic medication use and the risk of gastroschisis: findings from the National Birth Defects Prevention Study, 1997-2007. Paediatr Perinat Epidemiol. 2013 Jul;27(4):340-5.

Genetics and Congenital Heart Defects
Congenital heart defects (CHDs) are the most common type of birth defect, affecting about one in every 100 babies born in the United States. Scientists are working hard to learn the causes of CHDs. Most CHDs are due to a complex relationship among environment, lifestyle, and genetic factors.
Using the genetic samples that NBDPS families provided, NBDPS researchers identified changes (sometimes called variants) in several genes that were linked with CHDs. Variants in four genes were found to increase the risk of heart defects. More research is needed to understand the functions of these genes and to confirm the study findings among different groups. This study is one of the first in NBDPS to study genes from babies and their mothers.
Li M, Cleves MA, Mallick H, Erickson SW, Tang X, Nick TG, Macleod SL, Hobbs CA; National Birth Defect Prevention Study. A genetic association study detects haplotypes associated with obstructive heart defects. Hum Genet. 2014 Sep;133(9):1127-38.

Fever in Pregnancy and Congenital Heart Defects
Fever in early pregnancy is common. It is reported by 5% to 10% of women during the first trimester. Congenital heart defects (CHDs) are the most common birth defect. NBDPS researchers looked to see if there is a link between fever during pregnancy and CHDs.
Among mothers of a baby without a birth defect, one out of 13 had a fever in early pregnancy. For mothers of a baby with a CHD, about one in 12 had a fever in early pregnancy. Researchers found that the risk for CHDs was higher if the fever was from a urinary tract infection or pelvic inflammatory disease than if it was from a respiratory, flu-like disease. The increased risk was seen for certain CHD types, such as heterotaxy and some obstructive heart defects. Results of this study suggest the risk for these heart defects might be lower in women who were taking multivitamins before their pregnancy.
Botto LD, Panichello JD, Browne ML, Krikov S, Feldkamp ML, Lammer E, Shaw GM; National Birth Defects Prevention Study. Congenital heart defects after maternal fever. Am J Obstet Gynecol. 2014 Apr;210(4):359.e1-359.e11.

Air Pollution and Congenital Heart Defects
Many pregnant women, especially those who live in urban areas, are exposed to different air pollutants. Although the Environmental Protection Agency sets air quality standards to limit the amount of pollution in our air, we still do not know whether the amounts of pollution women are exposed to can affect their unborn babies.
NBDPS researchers found that higher exposure to air pollutants related to car traffic, specifically nitrogen dioxide, was more common among mothers of babies born with certain types of congenital heart defects (CHDs). More research is needed to learn what levels of air pollution affect an unborn baby.
Stingone JA, Luben TJ, Daniels JL, Fuentes M, Richardson DB, Aylsworth AS, Herring AH, Anderka M, Botto L, Correa A, Gilboa SM, Langlois PH, Mosley B, Shaw GM, Siffel C, Olshan AF; National Birth Defects Prevention Study. Maternal exposure to criteria air pollutants and congenital heart defects in offspring: results from the national birth defects prevention study. Environ Health Perspect. 2014 Aug;122(8):863-72.

The Potential Impact of Newborn Pulse Oximetry Screening
In the United States, about 7,200 babies born each year have critical congenital heart disease, also known as CCHD. CCHDs are the most serious types of congenital heart defects (CHDs). CCHDs often lead to low levels of oxygen in a newborn. A low oxygen level in a baby can be found by testing oxygen levels 24 hours after birth.
NBDPS researchers found that about 30% of the babies with CCHDs were diagnosed more than three days after birth. The percentage of babies with more than three days delay in diagnosis varied based on CCHD type—ranging from about 8% for babies with pulmonary atresia to 62% for babies with coarctation of the aorta. If these babies had been tested for CCHD within 24-48 hours of birth, as is now mandated in many state newborn screening programs, some of them might have been diagnosed sooner, leading to earlier treatment.
Peterson C, Ailes E, Riehle-Colarusso T, Oster ME, Olney RS, Cassell CH, Fixler DE, Carmichael SL, Shaw GM, Gilboa SM; National Birth Defect Prevention Study. Late detection of critical congenital heart disease among US infants: estimation of the potential impact of proposed universal screening using pulse oximetry. JAMA Pediatr. 2014 Apr;168(4):361-70.

Risk Factors for Choanal Atresia in the NBDPS
Choanal atresia is a narrowing of the nasal airway and can cause severe breathing problems in newborns. It is one of the leading causes of nasal surgery. Choanal atresia is rare, and not much is known about its risk factors. NBDPS researchers looked for reasons that might increase the risk for having a baby with choanal atresia.
Researchers found that the risk of choanal atresia was higher when women smoked cigarettes, had three or more cups of coffee with caffeine every day, or used thyroid medications early in their pregnancy. This study is one of the first to look at risk factors for choanal atresia, so more research is needed to confirm these findings.
Kancherla V, Romitti PA, Sun L, Carey JC, Burns TL, Siega-Riz AM, Druschel CM, Lin AE, Olney RS; National Birth Defects Prevention Study. Descriptive and risk factor analysis for choanal atresia: The National Birth Defects Prevention Study, 1997-2007. Eur J Med Genet. 2014 Apr;57(5):220-9.

Participation in the Genetic Component of NBDPS
Most women (63%) who finished an NBDPS phone interview also gave NBDPS genetic samples by providing swabs of their cheek cells. NBDPS researchers found that taking part in the genetics part of the study differed by Center. The participation ranged from 50% to 74% across different sites.
Participation also differed by race/ethnicity. Among white and Hispanic women, those with a higher education and had a baby with a birth defect were more likely to complete the cheek cell collection than women of other races. Among all racial/ethnic groups, an extra $20 incentive and a shorter time between the baby’s due date and the phone interview were linked with women being more likely to participate. Researchers can use this feedback to increase participation in similar studies in the future.
Glidewell J, Reefhuis J, Rasmussen SA, Woomert A, Hobbs C, Romitti PA, Crider KS; National Birth Defect Prevention Study. Factors affecting maternal participation in the genetic component of the National Birth Defects Prevention Study-United States, 1997-2007. Genet Med. 2014 Apr;16(4):329-37.

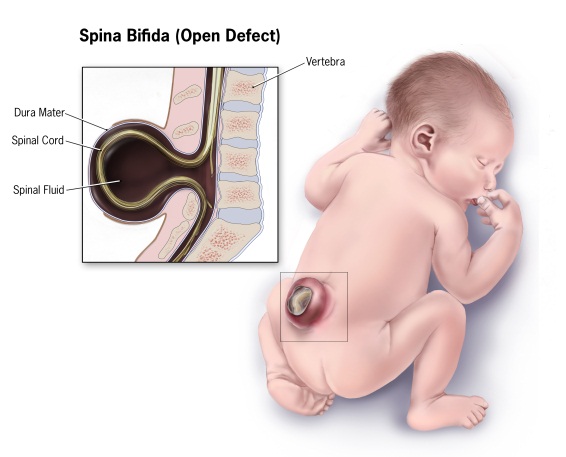
Obesity as a Risk Factor for Birth Defects
Background: Persons are obese if their weight is greater than what is generally considered to be healthy for their height. Whether or not someone is obese is determined using their height and weight in a calculation called body mass index (BMI). In the United States, more than half of women aged 20 to 39 years are overweight (BMI from 25 to 29.9) or obese (BMI 30 or more). Previous studies have suggested that a woman’s BMI before pregnancy might affect her risk of having a baby with certain birth defects. NBDPS researchers looked at whether a mother’s weight before pregnancy was linked with an increased risk for 16 categories of major birth defects.
Findings:
• This study confirmed that obese mothers are about twice as likely to have a baby affected by spina bifida than mothers who are a healthy weight (BMI between 18.5 and 24.9) at the start of pregnancy.
• Overweight and obese mothers also are at a slightly higher risk of having a baby affected by a congenital heart defect than mothers who are a healthy weight.
• Reaching and maintaining a healthy weight can help reduce these risks.
Waller DK, Shaw GM, Rasmussen SA, Hobbs CA, Canfield MA, Siega-Riz AM, Gallaway MS, Correa A. Prepregnancy obesity as a risk factor for structural birth defects. Archives of Pediatrics & Adolescent Medicine. 2007; 161(8):745-750.
Antidepressant Medications and Birth Defects
Background: Depression in women is most common during childbearing years. Selective serotonin-reuptake inhibitors, or SSRIs, are increasingly used to treat depression in pregnant women. Examples of medicines that are SSRIs include Prozac (fluoxetine), Zoloft (sertraline), and Paxil (paroxetine). We don’t know whether it is safe for pregnant women to use SSRIs, so NBDPS researchers looked for a possible link between taking these medicines during pregnancy and birth defects.
Findings:
• SSRI use during pregnancy did not increase the risk for most birth defects studied, including heart defects. Overall, these results were reassuring.
• SSRIs were linked to a small increase in risk for three birth defects: anencephaly , craniosynostosis , and omphalocele , but these findings have not been confirmed in other studies.
• Women should talk with their doctor about the best options for management of their depression during pregnancy.
Alwan S, Reefhuis J, Rasmussen SA, Olney RS, Friedman JM. Use of selective serotonin-reuptake inhibitors in pregnancy and the risk of birth defects. New England Journal of Medicine. 2007; 356(26):2684-92.

Diet Quality and Neural Tube Defects (NTDs) and Orofacial Clefts
Background: In the past, single nutrients (such as the amount of each vitamin in the diet) have been studied to see if they affect a woman’s risk of having a child born with a birth defect. To expand beyond looking only at one vitamin or nutrient at a time, NBDPS researchers studied whether the overall quality of a woman’s diet is linked to a lower risk of some birth defects. For example, researchers scored women’s diet quality by looking at those who followed a Mediterranean diet consisting of a lot of fish, beans, and vegetables as well as those who followed the U.S. food guide pyramid.
Findings: Women with a healthier diet (women who received better scores in their diet quality) in the year before pregnancy had a lower risk of having a baby with either a neural tube defect (NTD), such as anencephaly and spina bifida, or cleft lip (with or without cleft palate).
Carmichael SL, Yang W, Feldkamp ML, Munger RG, Siega-Riz AM, Botto LD, Shaw G. Reduced Risks of Neural Tube Defects and Orofacial Clefts With Higher Diet Quality. Archives of Pediatrics and Adolescent Medicine. 2012; 166(2):121-126.

Cooking and Grilling By-Products as a Risk Factor for Gastroschisis
Background: Polycyclic aromatic hydrocarbons (PAHs) are chemicals that are released when fuel is burned or when meat is cooked or grilled. A link between exposure to PAHs during pregnancy and having babies born with gastroschisis has been found in animal studies, but not in studies of humans. Therefore, NBDPS researchers looked at this potential link in humans.
Findings:
• Exposure at work to PAHs might increase the risk of having a baby with gastroschisis among mothers older than 20 years.
• Further study of this exposure and its potential link to birth defects is needed to confirm or refute this preliminary finding.
Lupo PJ, Langlois PH, Reefhuis J, Lawson CC, Symanski E, Desrosiers TA, Khodr ZG, Agopian AJ, Waters MA, Duwe KN, Finnell RH, Mitchell LE, Moore CA, Romitti PA, Shaw GM. Maternal occupational exposure to polycyclic aromatic hydrocarbons: effects on gastroschisis among offspring in the National Birth Defects Prevention Study. Environmental Health Perspectives. 2012; 120(6):910-915.

Folic Acid and Diabetes Associated Birth Defects
Background: Diabetes is a condition in which a person’s body cannot use the sugars and starches(carbohydrates) contained in foods to make energy. Previous studies have shown that women with poor control of diabetes (high or low blood sugar) during pregnancy have a higher risk of having a baby with a birth defect or other health problems. There can also be serious complications for the mother. NBDPS researchers examined whether or not taking vitamins containing folic acid (one of the B vitamins) before and during early pregnancy changed the risk of having a baby with a birth defect among women who already had diabetes.
Findings:
• Babies born to mothers with diabetes who did not take a vitamin containing folic acid might be at increased risk for birth defects compared with babies born to mothers with preexisting diabetes who did take a vitamin containing folic acid before and during early pregnancy – meaning, the vitamin containing folic acid seems to help lower the risk of birth defects for women with diabetes.
• The findings in this study are only preliminary because there was a relatively small number of mothers who had diabetes before pregnancy that did not use vitamins or supplements that contained folic acid. In addition, we did not have information on how well these women kept their blood sugar within the healthy range (their level of diabetes control), which is an important factor that affects the risk of birth defects.
Correa AF, Gilboa SM, Botto LD, Moore CA, Hobbs CA, Cleves MA, Riehle-Colarusso TJ, Waller DK, Reece EA. Lack of periconceptional vitamins or supplements that contain folic acid and diabetes mellitus-associated birth defects. American Journal of Obstetrics and Gynecology. 2012; 206(3):218.e1-218e.13..

Neural Tube Defects (NTDs) and Folate Intake among Pregnancies Conceived after Folic Acid Fortification in the United States
Background: Previous studies have shown that women with diets high in folate, the natural form of the B vitamin, folic acid, have a lower risk of having a baby with a neural tube defect. There are two easy ways to be sure to get enough folate each day: take a vitamin that has folic acid in it or eat cereal grain foods containing folic acid. The addition of folic acid to cereal grains (like breads and breakfast cereals), known as folic acid fortification, was fully implemented in the United States by 1998. Each year folic acid fortification prevents about 1,000 neural tube defects (NTDs). Therefore, the occurrence of NTDs has decreased since the United States began fortifying foods with folic acid. In this study, NBDPS researchers looked at whether women’s intake of folic acid from both vitamin pills/supplements and from their diet affected the risk of NTDs after fortification was required in the United States.
Findings:
• During the time of the study (1998 – 2003), which was after fortification of U.S. foods with folic acid had started, a mother’s risk of having a baby with a neural tube defect was not linked with the mother’s folic acid intake from either vitamin pills/supplements or from her diet.
• One possible explanation is that folic acid fortification prevented the NTDs that would have otherwise been caused by a lack of folic acid.
• Although folic acid fortification appears to benefit the majority of pregnant women in the United States, there might be some sub-populations, such as obese women or Hispanic women, who still have an increased risk of having a baby with a folic acid-preventable NTD.
• Further research is needed to study these sub-populations that may still have an increased risk.
Mosley BS, Cleves MA, Siega-Riz AM, Shaw GM, Canfield MA, Waller DK, Werler MM, Hobbs CA. Neural tube defects and maternal folate intake among pregnancies conceived after folic acid fortification in the United States. American Journal of Epidemiology. 2009; 169(1):9-17.
Exposures during a Father’s Job and Birth Defects
Background: Most birth defects are thought to be due to things that a woman comes into contact with, like the food she eats or the medicine she takes, just before or during her pregnancy. However, some things that the father comes into contact with before a baby is conceived might also affect the risk of having a baby with a birth defect, particularly if the exposure (for example, pesticides or paint fumes) affect the father’s sperm or fertility. Recently, NBDPS researchers looked at different exposures during work that might increase the risk of fathers having a baby with a birth defect. Investigators grouped hundreds of job types into many categories.
Findings:
• The strongest link was seen between working as an artist and birth defects of the mouth, eyes, ears, digestive system, limbs, and heart.
• A father’s job as a photographer, photo processor, or motor vehicle operator might increase the risk for certain eye defects.
• Working as a landscaper or groundskeeper was linked with certain birth defects of the digestive system. • These increased risks for certain jobs were relatively small and were based on small numbers. • More studies are needed to understand which exposures for fathers might increase the risk of birth defects in their babies.
Desrosiers TA, Herring AH, Shapira SK, Hooiveld M, Luben TJ, Herdt-Losavio ML, Lin S, Olshan AF, and the National Birth Defects Prevention Study. Paternal occupation and birth defects: findings from the National Birth Defects Prevention Study. Occup Environ Med. 2012 Aug;69(8):534-42.
